Exercise advice following gynaecological, bladder and pelvic floor surgery
This page aims to help guide you through your recovery from gynaecological surgery.
What can I expect after surgery?
Following your operation, you may have difficulty or discomfort carrying out normal activities. Your operation may have been performed through your abdomen (tummy), your vagina (birth canal) or laparoscopically (key hole). The time it takes to recover after these different types of surgery will vary dependent on your age, lifestyle and fitness levels. We therefore recommended that you practice the exercises listed on this page before your surgery.
Length of stay
You will usually be admitted to hospital on the day of your operation. Most women go home between 2 and 4 days after their operation but it may be sooner if you have had laparoscopic surgery.
What to do when you wake up from your surgery
Get up and move around. It will help with your recovery if you walk short distances as soon as you are able to.
You can avoid complications from surgery such as pneumonia, blood clots and muscle weakness by starting the exercises on the next page:
- Leg exercises
- Rotate your feet to the right and left.
- Wiggle your toes and bend your feet up and down.
- Stretch your legs out straight.
Repeat these exercises 4 to 5 times every half hour while you are awake.
- Deep breathing exercises
- Sit upright and take a deep breath to the bottom of your lungs. Allow your tummy to rise and feel your lower ribs move outwards.
Repeat at least 10 times every waking hour.
Repeat every hour that you are awake or every time you need to cough.
- Getting out of bed with assistance
- Roll onto your side.
- Push up with your hands.
- Lower your feet over the side of the bed.
- If you have stitches in your tummy you may want to give some extra support by holding onto your tummy with a rolled towel or your hands as you come forwards.
- Get up and walk regularly with assistance
- Walk with assistance until you feel confident to walk independently.
Toilet advice
It will help your bladder and your bowels if you drink normally (1.5 to 2 litres per day). See our ‘Fluid and caffeine intake for bladder and bowel health GHPI0533’ leaflet for more information.
A urinary catheter may have been inserted into your bladder during surgery. Once this has been taken out and you can use the bathroom, please try to sit properly on the toilet.
Take your time and relax using 5 or 6 long slow deep breathes to help you. Ideally, you should be passing urine every 3 to 4 hours during the day time.
If you are having any difficulties passing urine or you are not getting the normal sensation of needing to go, please tell your nurse or doctor immediately.
Try to avoid getting constipated after your surgery as this can put extra strain through both your pelvic floor muscles and the cuts made for your surgery. Drinking enough fluids will help as will eating plenty of vegetables, fruit and fibre. Discuss whether you need laxatives with your nurse or doctor before you go home.
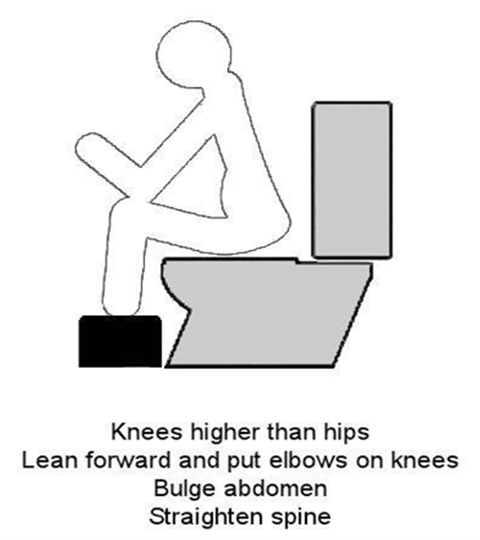
The correct position for opening your bowels
Sitting in the correct position on the toilet will make it easier for you to empty your bowel. Follow the steps below to get into the most effective position.
Step 1
Sit on the toilet and raise your feet onto a foot rest (a stool or even a pile of books will do). The aim is for your knees to be higher than your hips.
Step 2
Lean forwards, with a straight spine, and rest your elbows on your knees.
Step 3
Bulge out your abdomen and pretend you are gently blowing out candles on a birthday cake. Rest and then do this again. Do not rush when emptying your bowels. Do not sit on the toilet for longer that 10 to 15 minutes and do not strain. You should be able to empty your bowel with very little effort.
If your stool is very hard it can be more difficult to pass and can even feel as if it has got stuck. The following technique can help:
- Hold something soft in your left hand such as a stress ball.
- Rest it on the left side of your tummy and put your right hand over the top.
- Rock yourself forward and rest, then rock yourself back and push out the stool.
- Try this for 5 to 10 minutes.
Remember: Make sure the toilet seat is comfortable (not too cold) and allow yourself enough time and privacy.
It is quite common for patients to feel more wind than usual after surgery. Getting out of bed and walking about will help it release.
For more information about improving bowel function and control, see our ‘Bowel Function and Control GHPI1412’ leaflet. Please visit www.gloshospitals.nhs.uk/our-services/services-we-offer/continence-service/
At home
You should continue to walk several times a day. You can gradually increase the distance and speed. The recommended daily exercise is half an hour each day. You should slowly build up to this. Many women are able to walk for 30 to 60 minutes after 3 to 4 weeks.
It is common to experience fatigue after surgery. Having a daily lie down and resting with your feet up can help. Increasing your walking has also been shown to improve fatigue.
Lifting
In order to stop putting strain on your pelvic area too soon after surgery, you should avoid lifting heavy objects such as shopping baskets, heavy roasting dishes, watering cans and small children for 3 months. This also applies to excessive stretching. You can start vacuuming and ironing 4 to 6 weeks after your surgery.
For prolapse surgery, please read the information leaflet you have been given by the surgical team.
Exercises to help your recovery
Pelvic floor exercises
The pelvic floor is a sling of muscles between your coccyx (tailbone) and your pubic bone. Its purpose is to maintain continence, support the pelvic organs and stabilise the pelvis.
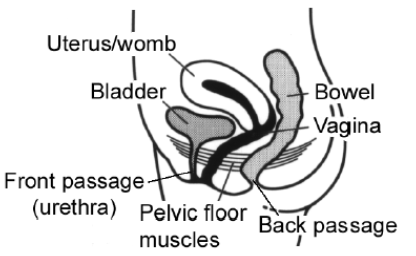
Pelvic floor muscles can weaken after pelvic surgery so it is important that you get them working again soon after your operation. This will help with your recovery and prevent problems in the future. Once the urinary catheter has been removed and you are passing urine normally it is safe to start gently exercising your pelvic floor muscles, even if you have stitches in the birth canal (vagina).
To contract the pelvic floor, gently squeeze around the back passage as if trying to stop wind and around your front passage as if you are trying to stop the flow of urine midstream. Hold this for as many seconds as you can (up to a maximum of 10 seconds). We recommended that 24 repetitions are performed daily. Try doing 8 holds, 3 times per day.
It is important to do the exercises in a variety of positions, for example, lying, sitting and standing to make sure that the muscle works well to support your pelvis. See our leaflet ‘Pelvic floor exercises for women GHPI0259_04_19’ for more information. Please visit www.gloshospitals.nhs.uk/your-visit/patient-information-leaflets/
You could also consider using an app such as Squeezy© to help you remember to do the exercises regularly. Squeezy© has been designed by chartered physiotherapists specialising in women’s and men’s pelvic health. Please visit www.squeezyapp.com for more information.
Abdominal exercises
- You should start to do gentle stomach exercises within the first few days after your operation.
- Start with the deep muscles (Stage 1) as they reduce the strain on your back and pelvic floor. Once this becomes easy to do, you can progress to working the outer muscles (Stage 2).
Stage 1: This exercises the deepest muscles of the stomach, which acts like a corset to stabilise your spine and pelvis and help flatten your stomach and draw in your waist-line.
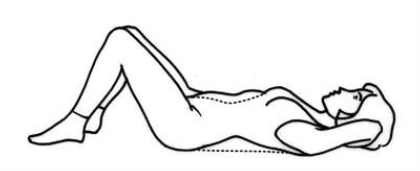
- Lie on your back with a pillow under your head, your knees bent and feet flat on the floor, see Figure 2.
- Let your tummy sag.
- Breathe in gently.
- As you breathe out, gently draw in the lower part of your stomach, towards the floor, squeezing your pelvic floor muscles at the same time.
Repeat this exercise 4 to 5 times, with a few seconds rest between each one. Aim to build up gradually, holding the muscles in for a maximum of 10 seconds and repeating up to 10 times in one go. You can do this exercise 2 to 3 times a day.
Stage 2: Once you are comfortably exercising the deep muscles, you can progress to the next stage of the programme.
The pelvic tilt
- Lie in the position shown (Figure 3) and perform the deep stomach exercises.
- Gently squeeze your pelvic floor and buttocks, tilt your pelvis up and flatten your back onto the floor or bed.
- Do not lift your bottom off the floor or bed.
- Hold this position for a maximum of 10 seconds.
- Release slowly.
- Repeat 4 to 5 times.
The head lift
- Perform a pelvic.
- Squeeze your pelvic floor muscles.
- As you breathe out, lift up your head only.
- Hold for a few seconds.
- Release slowly.
- Rest for a few seconds.
- Repeat 4 to 5 times.
Once you feel confident with the head lift you can progress by:
- Prolonging the hold, up to a maximum of 10 seconds.
- Raising your head and shoulders.
- Repeat 2 to 3 times a day.
Remember
- Tighten your pelvic floor muscles as you do the exercise.
- Breathe out as you contract your muscles.
- It may take several weeks before you progress to this stage; this is nothing to worry about.
Returning to normal activities
Recovery varies from person to person and your return to normal activity should be gradual.
For the first 6 weeks to help your healing and avoid straining the surgery and your pelvic floor:
- Start your pelvic floor exercises.
- Start your abdominal exercises.
- Walk every day, starting with little and often to build on the distances you managed in hospital.
- Do not stand for more than 30 minutes at a time.
- Minimise lifting as much as possible.
- Listen to your body
Resuming sports
Try low impact exercise such as low-level Pilates, cross trainer, more vigorous walking, gentle aerobics from about 6 weeks. You will need to wait until any vaginal discharge and bleeding has stopped before starting these exercises.
Swimming
This can usually be resumed within 2 to 3 weeks, as long as any vaginal bleeding and discharge has stopped.
Contact/high intensity sport
These should be avoided for at least 8 to 12 weeks. If you have had surgery to repair a prolapse, please see the information leaflet you have been given by the surgical team.
Driving
Before you return to driving you must feel able to concentrate and to carry out an emergency stop without any pain or discomfort in your pelvic area. You should be comfortable wearing a seatbelt and be able to turn to look over your shoulder. You should start with short journeys.
Contact your insurance company to find out when you are covered to start driving again. Their rules on this can vary.
Having sex
You should usually allow 4 to 6 weeks after your operation for your scar to heal. It is then safe to have sex, as long as you feel comfortable. If you experience any discomfort or dryness, you may wish to try a vaginal lubricant. Think about using positions where you are more able to control the amount of penetration.
If you have any ongoing issues, please ask your GP for advice. Alternatively, you can self-refer to see a physiotherapist; visit www.gloshospitals.nhs.uk and type in ‘physiotherapy self-referral’ for more information.
Returning to work
Everyone recovers at a different rate, so when you are ready to return to work will depend on the type of work you do, the number of hours you work and how you get to and from work. You should aim for a graded return to work with a gradual increase in your hours and activity.
Contact information
Recovering from an operation is a very personal experience. If you need further advice, you can contact a women’s health physiotherapist:
Cheltenham General Hospital
Tel: 0300 422 2345 (answerphone)
Gloucestershire Royal Hospital
Tel: 0300 422 8303 9 (answerphone)
Please leave a message and we will try to get back to you within 5 working days.
Email: ghn-tr.womenshealth.physio@nhs.net
Website: www.gloshospitals.nhs.uk/our-services/services-we-offer/physiotherapy/how-can-i-see-physiotherapist/